COVID Case Report
E.RISHITHA REDDY
ROLL.NO-30
“This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome."
I've been given this case, in an attempt to understand the topic of "patient clinical data analysis" and to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations as well as to come up with a diagnosis and treatment plan.
All the information was obtained from the patient's relative, along with inputs from Dr. Praneeth Reddy sir (PG) and under the guidance of Dr. Rakesh Biswas sir.
. Abstract
We presently report the case of COVID-19 in a 50-year-old-female who had come to the hospital. She reported having currently no complaints.symptomatically saturation’s have been fluctuating 86-92% on room air. On presentation, PR-79bpm SpO2-92% on RA.she was advised admission in hospital. However ,The result of PCR for COVID-19 RNA was positive.
Case Report
A 50-year-old female, who had come to hospital.
History of presenting illness-
presented with a chief complaint of fever 8 days back. she gives no other complaints of breathlessness , cough, fatigue, loss of taste and smell. And was tested to be Rapid Antigen positive for COVID-19 3days back and was admitted on 1/5/21 and discharged on 7/5/21.
And again she presented back to hospital with complaints of saturation’s fluctuating between 86-92% on RA
PAST HISTORY:
She is not a known case of DM,HTN
PERSONAL HISTORY
Diet: Mixed
Appetite: Normal
Sleep: Disturbed
Bowel, bladder: Regular
No addictions
DRUG HISTORY
No known drug allergies.
FAMILY HISTORY
No significant Family history.
None of his family members are tested COVID positive
GENERAL EXAMINATION
The patient is conscious, coherent, cooperative and well oriented to time place and person
She is sitting comfortably on the bed. She is moderately built and well nourished
PALLOR - Absent
ICTERUS - Absent
CYANOSIS - Absent
CLUBBING- Absent
LYMPHADENOPATHY -Absent
EDEMA - Absent
VITALS AND INVESTIGATIONS:
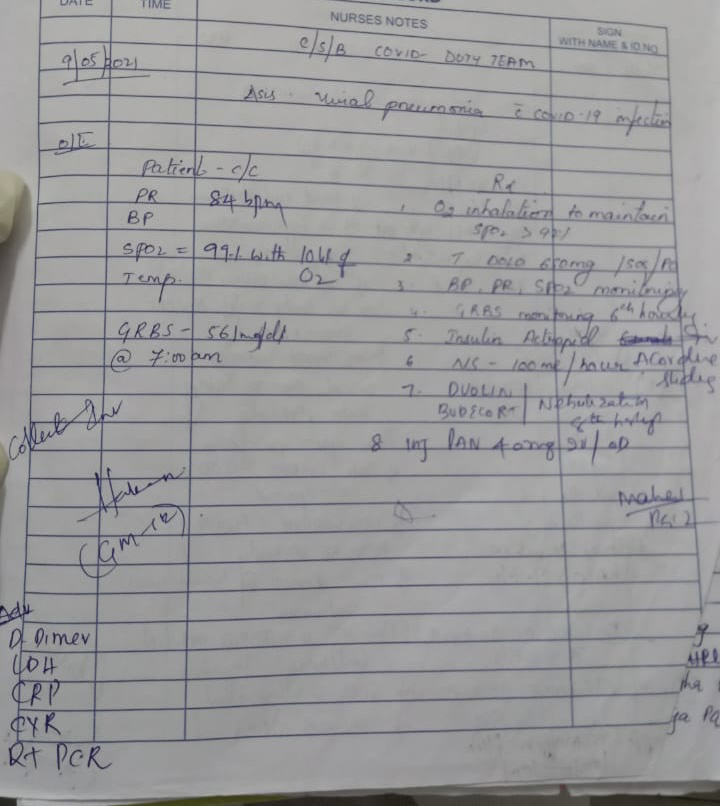
On 9/5/21:
On physical exam,
she was stable,
temperature was 36.5°C,
respiratory rate was 16,
pulse rate was 84, and
O2 saturation was 99% and
GRBS-561mg/dl @7:00a.m.(high grbs levels)
Investigations Advised:
-D- dimer
-LDH
-CRP
-CXR
-RT-PCR
On 10/5/21:
On physical examination her
PR-80 bpm
BP-110/70
SpO2-99%
RR-30/min
Temp-97F
Investigations reports of 9/5/21:
LDH-409.2(elevated)
D-dimer-460ng/ml(elevated)
GRBS-326mg/dl(elevated))
Wt
Alb+
Sug +++
Pus cells -3-6 cells
Epi cells -2-4 cells
Ketones- negative
HbA1c -7.9%(elevated)
On 11/5/21:
On physical examination her :
PR-80 bpm
BP-110/70 mm of hg
SpO2-98%
RR-24/min
Temp-97.4F
Advised-at 6’O clock
-CBP
-CRP
-D-dimer
-spectrum of AFB
On 12/5/21:
On physical examination her
Patient-conscious and coherent
PR-80 bpm
BP-110/70
SpO2-99%
RR-30/min
Temp-97F
Investigations reports
GRBS-238mg/dl@8am
377mg/dl@1pm
286mg/dl@8pm
Advised-
-HRCT
On 13/5/21:
On physical examination her
Patient-conscious and coherent
PR-94 bpm
BP-120/60 mm of hg
SpO2-99%
RR-30/min
Temp-97F
Poor oral hygiene
Investigations reports :
GRBS-310mg/dl@8am
375mg/dl@1pm
238mg/dl@8pm
On 14/5/21:
On physical examination her
Patient-conscious and coherent
PR-78bpm
BP-120/60 mm of hg
SpO2-97% with bht of O2
RR-30/min
Temp-97F
Poor oral hygiene
Investigations reports :
GRBS-238mg/dl @8am
VITALS:
Record of patients vitals :
BP
PULSE
TEMPERATURE
SpO2
GRBS
SYSTEMIC EXAMINATION
RS - Normal vesicular breath sounds heard
CVS- s1 and s2 heard. No added murmurs
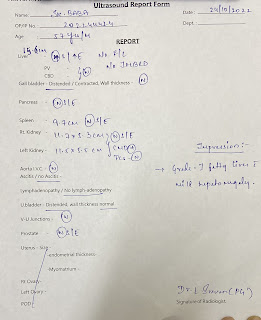
PA- Soft and non tender. No organomegaly
CNS- Intact
LOCAL EXAMINATION
No external injuries or scars seen
INVESTIGATIONS
REPORTS FROM HOSPITAL-
1. General investigations-
CBP, CRP, RFT, LFT,LDH.
CBP-
CRP-
RFT-
LFT-
LDH-
ECG report:
Urine examination for ketone bodies-
HbA1C-(glycated hemoglobin)-
SUMMARY OF INGESTIGATIONS
TRP GRAPHIC CHART:
Provisional Diagnosis
Viral pneumonia secondary to COVID of a denovo Diabetes Mellitus .
Rx-
1.head end elevation
2.O2 supplementation if SpO2<95%
3.Tab.DOLO 650 mg/PO/SOS
4.Tab.PANTOP 40 mg/PO/BBF
Same *~*
6.Tab. LIMCEE /PO/OD
—— *2pm*——
7.Nebulisation with Duolin and budecort 8th hrly
8.IVF-NS@ 100 ml/hrly continuous
9.on inj.H.ACTRAPID insulin 6ml/hrly infusion
10.GRBS charting hrly
11.MONITOR VITALS
12.Tab.OSELTAMIVIR 75 mg BD
13.Inj. CLEXANE 40 mg
S.C / OD
14.Syp.Cremaffin-plus
10 ml — 10 ml
15.BP,PR,SpO2 monitoring
16.2%betadine mouth gargle diluted with water 4-5 times /day




























Comments
Post a Comment