This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
Chief complaints:
C/o of constipation since 20 days
C/o of fever since 4 to 5 days
History of presenting illness:
patient came with c/o of constipation since 20 days I was admitted in hospital for three days
C/o of fever high-grade since 4 to 5 days more during night
history of hiccups 15 days back admitted in hospital for three days
no c/o of decreased urine output vomiting headache
chief complaints of decreased appetite since 5 to 6 days
History of past illness :
history of giddiness accident 8/6 starring went to hospital and scan was done
K/c/o hypertension since 1 1/2 year on medication
Not a k/c/o diabetes mellitus TB epilepsy CAD asthma
Personal history :
appetite - lost
diet - mixed
bowels - constipation
micturition - normal
no known allergies
addictions :
alcohol since 27 years stop at one month back
smoking since 27 years stop and 15 days back
Family history : no significant family history
General examination :
no Pallor ,icterus, cyanosis, clubbing ,lymphadenopathy, Edema, Mal nutrition
Temperature -afebrile
pulse rate- 64 BPM
BP-110/70mmHg
SPO2-94%
GRBS- 124mg /dl
Cardiovascular system :
S1 S2 heard
no cardiac Murmurs
Respirator system :
no dyspnoea
no wheeze
trachea position Central
breath sounds vesicular
CNS:
No focal and neurological deficits
Upper limb lower limb
Rt left Rt left
Tone normal normal increased increased
Power 5/5 5/5 5/5 5/5
Reflexes right left
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle
Plantar flexion Flexion
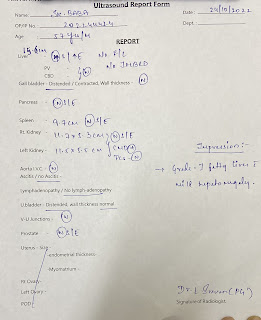
Usg:
Chest xray:
X-ray erect abdomen :
Ecg:
Provisional diagnosis:
Uremic encephalopathy with Alchohol dependence syndrome with AKI with h/o CVA with k/c/o
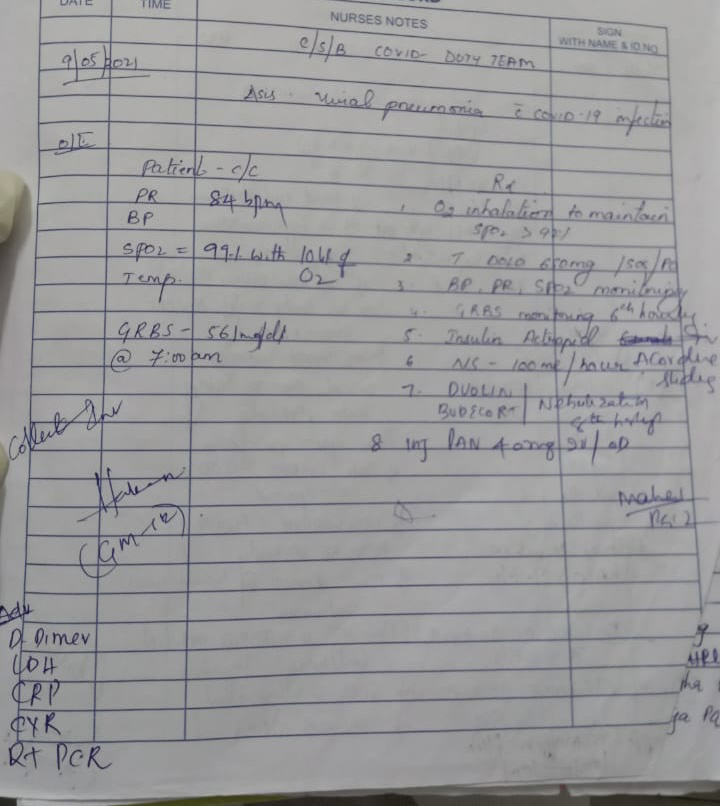
Rx:
1.Inj.MONOCEF 1gm IV STAT
2.IV FLUIDS DNS@50 ml /hr
3.INJ.THIAMINE 200mg IV TID in 100 ml NS over 30 mins
4.SYP LACTULOSE 15ml PO BD
5.MONITOR VITALS











Comments
Post a Comment