ONLINE BLENDED BIMONTHLY ASSESMENT-MAY
I have been given the following cases to solve in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
A 55 year old female patient, a resident of Miryalaguda and farmer by occupation came to the hospital on 17/5/21 with the chief complaints of shortness of breath, pedal edema and facial puffiness.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY-
OTHER SYMPTOMS-
5 yrs ago-Anaemia
1 month back-Generalised weakness
20 days ago- Hypertension
15 days ago- pitting type of pedal edema and facial puffiness
ANATOMICAL LOCALISATION OF THE PROBLEM-
Bronchi and bronchioles of the lung
PRIMARY ETIOLOGY OF THE PROBLEM-
HERE THE ALLERGEN IN THIS CASE IS THE RICE DUST.
THIS ALLERGEN TRIGGERS THE LYMPHOID TISSUE AND THE PLASMA CELLS TO RELEASE THE IgE WHICH CAUSES THE IgE TO BIND TO THE MASTCELLS AND RELEASES THE HISTMINE AND BRADYKININ.THIS CAUSE THE NARROWING OF THE RESPIRATORY TRACT BY INCREASING THE MUCOUS PRODUCTION .
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1.Head and elevation: Significantly increases global and regional end-expiratory lung volume. It has also been shown to improve oxygenation and hemodynamic performance.
2.Bipap intermittent: By having a custom air pressure for when you inhale and a second custom air pressure when you exhale, the machine is able to provide relief to your overworked lungs and chest wall muscles.
3.inj.Augmentin
Augmentin is a prescription antibiotic medication. It’s used to treat infections caused by bacteria. It belongs to the penicillin class of antibiotics. It contains two drugs: amoxicillin and clavulanic acid. This combination makes Augmentin work against more types of bacteria than antibiotics that contain amoxicillin alone.It is effective for treating infections caused by many different types of bacteria. These include bacteria that cause:
pneumonia, ear infections, sinus infections,skin infections,urinary tract infections
4. Tab Azithromycin antibiotic
5. Inj lasix
6.Tab pantop
It is commonly used for the diagnosis or treatment of Gastro-esophageal reflux disease, Heartburn, Euophagus inflammation, Stomach ulcers.
7.Inj.Hydrocortisone
It is used to treat disorders of the skin, hormones, stomach, blood, nerves, eyes, kidneys, or lungs. They also include rheumatic disorders, allergic problems, certain cancers, or problems with the intestines such as ulcerative colitis.
8.Nebuliser with
A) ipravent: It is an anticholinergic bronchodilator. It is used in the Treatment of COPD and prevention of asthma
B)budecort: It is a corticosteroid and acts as an anti-asthmatic agent. It helps in controlling daily symptoms such as shortness of breath, wheezing and chest pain and prevents the worsening of these symptoms. Budecort should always be administered with the help of nebulisers. Nebuliser is a machine that forms a mist of medicine so that it can reach the lungs easily. Your doctor or pharmacist will guide you on how to use nebulisers properly. You should take Budecort regularly as advised by your doctor for effective control of your asthma
9. Tab pulmoclear
It contains a combination of two medicines, Acebrophylline and Acetylcysteine. They belong to the class of bronchodilators and mucolytics, respectively. It is used for relieving the symptoms of coughing, wheezing, congestion and blockage in the airways in a condition called chronic obstructive pulmonary disease (COPD).
10) Chest physiotherapy
It is a term used for a group of treatments designed to improve respiratory efficiency, promote expansion of the lungs, strengthen respiratory muscles, and eliminate secretions from the respiratory system.It includes postural drainage, chest percussion, chest vibration, turning, deep breathing exercises, and coughing.
11)Inj HAI SC
Human Actrapid 40IU/ml Solution for Injection is a short-acting insulin used to treat type 1 and type 2 diabetes mellitus. It is used together with a healthy diet and regular exercise to control blood sugar levels after meals. This helps to prevent serious complications of diabetes like kidney damage and blindness.
12) Inj thiamine
To treat or prevent thiamine(B1) insufficiency
13)Vitals charting
This allow for continuous monitoring of a patient, with medical staff being continuously informed of the changes in general condition of a patient.
14)I/O chartUrine input/output chart
This chart (also known as a frequency-volume chart or bladder diary) is used to assess how much fluid you drink, to measure your urine volume, to record how often you pass urine over 24 hours and to show any episodes of incontinence (leakage)
15) O2 inhalation
It is used to
A) manage the condition of hypoxia
B)maintain o2 tension in blood plasma
C)increase oxy haemoglobin in RBC
D) maintain ability of cells to carry out normal metabolic function
E)reduce the risk of complications
3) What could be the causes for her current acute exacerbation?
Allergens, e.g., pollens, wood or cigarette smoke, pollution Toxins, including a variety of different chemicals
4. Could the ATT have affected her symptoms? If so how?
There are some case reports about interstitial lung disease (ILD) such as pneumonitis caused by isoniazid (INH), rifampin (RFP), ethambutol (EMB). Therefore The causative drug was discontinued permanently or re-administrated after desensitization therapy.
5.What could be the causes for her electrolyte imbalance?
The distribution of electrolyte disturbances in COPD group (total 58.53%) was found as follows: hypokalemia in 20%, hyponatremia in 13.33%, hypomagnesemia in 6.66%, hypochloremia in 3.33%, and combined disturbances in 15%.
Activation of the renin-angiotensin-aldosterone system and inappropriately elevated plasma arginine vasopressin in COPD may aggravate the electrolyte imbalance during acute exacerbation of COPD
This patient has Hyponatremia and Hypochloremia according to the reports
Hyponatremia in patients with COPD developed secondary to many reasons, such as development or worsening of hypoxia, hypercapnia, and respiratory acidosis, and right-side heart failure with development of lower limb edema, renal insufficiency, use of diuretics respiratory acidosis with metabolic alkalosis (owing to renal compensation) in patients with COPD with chronic hypercapnia is the usual cause of hypochloremia in those patients.
CASE2-
A 40 year old male presented to the hospital from Yadagirigutta with the chief complaints of irrelevant talking and decreased food intake since 9 days.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
He was unable to lift himself off the bed and move around, and had to be assisted. It was associated with a decrease in food intake since 9 days.
he had 2-3 episodes of seizures, one being 1 year ago
most recent being 4 months ago.
most recent time, (4 months ago), he had developed seizures (most probably GTCS) following cessation of alcohol for 24 hours, which was associated with restlessness, sweating, and tremors
9 days back-The patient started talking and laughing to himself
ANATOMICAL LOCALISATION-
withdrawal seizures are triggered by neuronal networks in the brainstem, including the inferior colliculus
Primary etiology:
Ethanol is the primary alcohol ingested by chronic users. It is a central nervous system (CNS) depressant that the body becomes reliant on with extended exposure to ethanol. It does this by inhibiting the excitatory portion (glutamate receptors) of the CNS and enhancing the inhibitory portions (GABA receptors) of the CNS. When the depressant is stopped, the central nervous system becomes overexcited as the inhibition is taken away. Thus, the body gets an excitatory overload, which results in the symptoms of withdrawal.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1.IVF NS and RL 150ml per hour:
aim of lowering alcohol levels and its metabolites, reducing its neuro-depressive effects, and making patents spending less time in the ED.
2.Thiamine:
Thiamine has no effect on the symptoms or signs of alcohol withdrawal or on the incidence of seizures or DTs. Routine use of thiamine is recommended because the development of Wernicke encephalopathy or Wernicke-Korsakoff syndrome is disastrous in these patients and can remain unrecognized. Because orally administered thiamine may have poor enteral absorption in individuals with alcoholism, high-risk patients should receive parenteral thiamine at 100-250 mg once daily for several days.
3.Lorazepam used to treat alcoholism and alcohol withdrawal symptoms. It is used by rehab facilities across the nation to help patients overcome an AUD.The drug helps alleviate anxiety associated with alcohol withdrawal. Treatment providers may also prescribe it to reduce the risk of seizures.
4.Pregabalin
Pregabalin is a high-affinity α2δ voltage-gated calcium channel subunit ligand indicated in different countries for the treatment of neuropathic pain associated with a variety of conditions, fibromyalgia, generalized anxiety disorder (GAD), and as adjunctive therapy for adults with partial-onset seizures
5.HAI
Human Actrapid 40IU/ml Solution for Injection is a short-acting insulin used to treat type 1 and type 2 diabetes mellitus. It is used together with a healthy diet and regular exercise to control blood sugar levels after meals. This helps to prevent serious complications of diabetes like kidney damage and blindness.
6.Lactulose
Lactulose is helpful in patients with an acute onset of severe encephalopathy symptoms and in patients with milder, chronic symptoms. This nonabsorbable disaccharide stimulates the passage of ammonia from tissues into the gut lumen and inhibits intestinal ammonia production.
8.Potchlor : Potklor liquid is used to treat low levels of potassium in the body
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
Alcohol tolerance is increased by regular drinking. This reduced sensitivity to the physical effects of alcohol consumption requires that higher quantities of alcohol be consumed in order to achieve the same effects as before tolerance was established
The first area compromised is the Cerebral Cortex, which causes confusion and lowers inhibitions. Next, it hits the cerebellum, altering movement and balance. If the user continues to drink, the hypothalamus and amygdala become affected. This may make it harder to control emotions If a user continues to drink at this point, it may affect the brain stem, which induces sleep and can cause irregular breathing and even seizures.
This might be the reasons why Neurological symptoms appeared later
4) What is the reason for giving thiamine in this patient?
A number of mechanisms may be involved in the pathogenesis of thiamin deficiency in the alcoholic population. An important cause is inadequate intake of thiamin. Moreover, there may be decreased convertion of thiamin to the active coenzyme, reduced hepatic storage of the vitamin in patients with fatty metamorphosis, ethanol inhibition of intestinal thiamin transport, and impaired thiamin absorption secondary to other states of nutritional deficiency.
5) What is the probable reason for kidney injury in this patient?
Mechanical ventilation was an important treatment for patients with AECOPD .On the contrary, mechanical ventilation was also an independent risk factor for AKI.
6). What is the probable cause for the normocytic anemia?
Anemia of chronic disease (ACD) is probably the most common type of anemia associated with COPD. ACD is driven by COPD-mediated systemic inflammation. Anemia in COPD is associated with greater healthcare resource utilization, impaired quality of life, decreased survival, and a greater likelihood of hospitalization. Anemia was normocytic and normochromic in nature.
The exact cause of anemia of chronic disease may vary. Anemia can be caused by a slight shortening of normal red blood cell survival. the production of red blood cells (erythropoiesis) or erythropoietin (a hormone that stimulates red blood cell production) may be impaired.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Oxygen is important for cell metabolism and is critical for all wound-healing processes
It inhibits wound healing by reducing the quantity and quality of oxygen to the wound site.
THIRD CASE-
B)https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
A 52 year old male came to the hospital 2 days back presenting with slurring of speech and deviation of mouth that lasted for 1 day and resolved on the same day.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
history of giddiness 7 days backstarted at around 7 am when the patient was doing his usual morning routine. He suddenly felt giddy and took rest, after which it subsided briefly. This was associated with 1 episode of vomiting on the same day.
- Patient was asymptomatic for 3 days, after which he consumed a small amount of alcohol.
- This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus.
- He has associated vomiting- 2-3 episodes per day, non projectile, non bilious containing food particles
Anatomical localisation
Cerebellum which is responsible for postural stability,ocular movements and vertigo(central)
Primary etiology:
usually results from damage to the part of your brain that controls muscle coordination (cerebellum). conditions can cause ataxia, including alcohol misuse, certain medication, stroke, tumor, cerebral palsy, brain degeneration and multiple sclerosis.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1.Vertin Tablet is used to prevent and treat a disorder of the inner ear known as Ménière's disease. The symptoms include dizziness (vertigo), ringing in the ears (tinnitus), and loss of hearing, probably caused by fluid in the ear. This medicine helps relieve the symptoms by reducing the amount of fluid.
2.Zofer anti-emetics' primarily used in the prevention of vomiting (being sick) and nausea (feeling sick) that usually occur after cancer chemotherapy, radiation treatment or surgery.
3.Ecosporin commonly used for the diagnosis or treatment of Headache, migraine, fever, sore throat, neuralgia
4.Atorvostatin
Statins are effective in reducing both first-ever and recurrent stroke, and this effect seems driven by the extent of LDL-C lowering
5.Clopidogrel is a type of medicine called an antiplatelet: it reduces the risk of blood clots forming within your circulatory system or blood vessels.
6.Mvt Methylcobalamin is used in vitamin B12 deficiency.
7.Methylcobalamin is a form of vitamin B12 that restores its level in the body thereby helping in treating certain anemias and nerve problems.
3) Did the patients history of denovo HTN contribute to his current condition?
Raised blood pressure (BP) is common after stroke but its causes, effects, and management still remain uncertain.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Ischemic stroke is the most common type of stroke. It is caused by a blood clot blocking the flow of blood and oxygen from reaching the brain.
A hemorrhagic stroke occurs either when an aneurysm bursts, or a weakened blood vessel leaks. The result is bleeding either inside the brain, causing an intracerebral hemorrhage, or, less commonly, bleeding between the brain and the tissue covering it, causing a so-called subarachnoid hemorrhage. heavy drinkers were about 1.6 times more likely to suffer from intracerebral hemorrhage and 1.8 times more likely to suffer from subarachnoid hemorrhage. The association between heavy alcohol consumption and these two types of stroke was stronger than that for ischemic stroke
Therefore, even if moderate drinking may have a beneficial effect by lowering the risk of ischemic stroke, the disadvantages might outweigh the benefits.
The adverse effect of alcohol consumption on blood pressure – a major risk factor for stroke – may increase the risk of hemorrhagic stroke and outweigh any potential benefit.
FOURTH CASE-
http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
45 years old female ,house wife by occupation came to opd with chief complaints of palpitations,chest heaviness,pedal edema,chest pain,radiating pain along her left upper limb , generalized body weakness
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
10 yrs back had the episode of paralysis of both upper and lowerlimbs (rt and left).
right and left paresis due to hypokalemia 1year back.
Swelling over the legs(bilateral)-8 months
blood infection -7 months back
2 months back for treatment of neck pain
6 days back pain along the left upper limb
5 days back chest pain ,difficulty in breathing ,and was able to feel her own heart rate.
Anatomical localization: Cervical spine
Primary etiology:
1.degenerative changes that occur in the cervical spine with age.
2.Dehydrated disks. Disks act like cushions between the vertebrae of your spine. By the age of 40, most people's spinal disks begin drying out and shrinking, which allows more bone-on-bone contact between the vertebrae.
3.Bone spurs. Disk degeneration often results in the spine producing extra amounts of bone in a misguided effort to strengthen the spine. These bone spurs can sometimes pinch the spinal cord and nerve roots.
4.Herniated disks. Age also affects the exterior of your spinal disks. Cracks often appear, leading to bulging (herniated) disks — which sometimes can press on the spinal cord and nerve roots.
5.Stiff ligaments. Ligaments are cords of tissue that connect bone to bone. Spinal ligaments can stiffen with age, making your neck less flexible.
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Reasons for recurrence :
The primary hypokalemic periodic paralysis is autosomal dominant and is exacerbated by strenuous exercise, high carbohydrate diet, cold and excitement, which was not found in this case. secondary periodic hypokalemic paralysis have been reported in association with gastroenteritis, diuretic abuse, renal tubular acidosis, Bartter syndrome, villous adenoma of colon, and hyperthyroidism.
Risk factors :
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
ECG changes include flattening and inversion of T waves in mild hypokalemia, followed by Q-T interval prolongation, visible U wave and mild ST depression in more severe hypokalemia.
FIFTH CASE-
A 55year old male patient came to opd with c/o altered sensorium and involuntary movements from 11pm and recurrent episodes of seizures since 5yrs.
1.Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Seizures after ischaemic strokes:
An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury
Seizures after haemorrhagic strokes:are thought to be attributable to irritation due to (hemosiderin Deposits)caused by products of blood metabolism
Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Initially the patient might have had Simple partial seizures (no loss of consciousness) and might have progressed to Generalised Tonic Clonic seizures (loss of consciousness).
SIXTH CASE
A 48-year-old gentleman hailing from a small town in Telangana presented to the casualty ward on 25th April 2021 at 7:40am with the chief complaints of unresponsiveness for 7 hours and 3 intermittent episodes of seizures in the past 3 hours
Questions:
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
The patient has minor unattended head injuries in the past 1 yr. According to the CT scan, the patient has cerebral hemorrhage in the frontal lobe causing probably for the occurrence of Frontal love ataxia
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
The patient has minor unattended head injuries. During the course of time the minor hemorrhages if present should have been cured on their own. But the patient is a chronic alchoholic. This might have hindered the process of healing or might have stopped the healing rendering it to grow further more into 13 mm sized hemorrhages occupying Frontal Parietal and Temporal lobes
SEVENTH CASE-
A 30 YEAR OLD MALE PATIENT WITH WEAKNESS OF RIGHT UPPERLIMB AND LOWERLIMB ,DEVIATION OF MOUTH TOWARDS LEFT
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
The closeness of facial bones to the cranium would suggest that there are chances of cranial injuries. Since the Zygomatic arch and Mandibular process is very close to the cranium, this might play a role in the patient's present condition
2.What are warning signs of CVA?
1.Weakness or numbness of the face, arm or leg, usually on one side of the body
2.Trouble speaking or understanding
3.Problems with vision, such as dimness or loss of vision in one or both eyes
4.Dizziness or problems with balance or coordination
5.Problems with movement or walking
6.Fainting or seizure
7.Severe headaches with no known cause, especially if they happen suddenly
3.What is the drug rationale in CVA?
1.Mannitol- Because of its osmotic effect, it is assumed to decrease cerebral edema.It might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
2.Ecospirin
For the prevention of heart attack, stroke, heart conditions such as stable or unstable angina (chest pain) due to a blood clot.
3.Atrovas-Atorva 40 Tablet belongs to a group of medicines called statins. It is used to lower cholesterol and to reduce the risk of heart diseases. Cholesterol is a fatty substance that builds up in your blood vessels and causes narrowing, which may lead to a heart attack or stroke.
4.Rt feed: RT feed is a nursing procedure to provide nutrition to those people who are either unable to obtain nutrition by mouth or are not in a state to swallow the food safely.
4. Does alcohol has any role in his attack?
When the patient met with an accident there might be cranial damage which was unnoticed.
If so his occasional drinking may or may not have hindered the process of the minor hemorrhages getting healed and might have caused this condition
But since the patient is not a chronic alcoholic and so Alcohol might not have played any role.
Therefore it cannot be evaluated without further details
5.Does his lipid profile has any role for his attack??
The inverse relationship between serum HDL-C and stroke risk . When taken together it seems clear that higher baseline levels of serum HDL-C lower the risk of subsequent ischemic stroke.
EIGHT CASE
50-year-old male patient presented to hospital with complaints of weakness of all four limbs since 8 PM yesterday.
*Questions*_
1)What is myelopathy hand ?
There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement
2)What is finger escape ?
This commonly results from weakness of some of the ulnar nerve innervated intrinsic hand muscles -in particular the palmar interosseous muscle to the little finger- caused by damage to their nerve supply (denervation).
In cervical myelopathy most commonly due to mechanical compression of the spinal cord in the neck as occurs in spondylitic cervical spinal stenosis but also seen in other spinal cord disease including post-traumatic tetraplegia. This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign”
3)What is Hoffman’s reflex?
The Hoffmann's reflex test itself involves loosely holding the middle finger and flicking the fingernail downward, allowing the middle finger to flick upward reflexively. A positive response is seen when there is flexion and adduction of the thumb on the same hand which can help verify the presence or absence of issues arising from the corticospinal tract.
A 17 year old female student by occupation presented to causality
Chief complaints of
1.Involuntary movements of both upper and lower limbs a day before.
1) What can be the cause of her condition ?
Presence of cortical vein thrombosis with hemorrhagic venous infarction in right posterior temporal lobe and also Iron deficiency anaemia
2) What are the risk factors for cortical vein thrombosis?
A)For children and infants
1.Problems with the way their blood forms clots
2.Sickle cell anemia
3Chronic hemolytic anemia
4.Beta-thalassemia major
5.Heart disease — either congenital or acquired
6.Iron deficiency
7.Certain infections
8.Dehydration
9.Head injury
B)For newborns, a mother who had certain infections or a history of infertility
1.For adults
2.Pregnancy and the first few weeks after delivery
3.Problems with blood clotting; for example, antiphospholipid syndrome, protein C and S deficiency, antithrombin III deficiency, lupus anticoagulant, or factor V Leiden mutation
4.Cancer
5.Collagen vascular diseases like lupus, Wegener’s granulomatosis, and Behcet syndrome
6.Obesity
7.Low blood pressure in the brain (intracranial hypotension)
8.Inflammatory bowel disease like Crohn’s disease or ulcerative colitis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
It may be any of the following reasons
1.Missed medication
2.Lack of sleep
3.Stress
4.Menstruation About half of women of childbearing age with epilepsy have increased seizures around their period. This is most likely due to hormonal changes that occur during your monthly cycle.
5.Herbal medications — as well as the herbs that go into many dietary supplements — can actually cause seizures or worsen side effects of seizure medication. The same goes with essential oils. Certain ones, such as juniper and umbrella plant, have been known to induce seizures.
6.Vitamin B6 (pyridoxine) deficiency is the only type of vitamin deficiency that’s been proven to potentially cause or worsen seizures
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Inj sodium valproate and Inj phenytoin have anti platelet activity. It can be used to prevent or remove already formed clots.
CARDIOLOGY-
FIRST CASE-
78 yr old male patient, resident of of kattangur and shepherd by occupation came to the Opd on 14 /5/2021 with chief complaints of :
SHORTNESS OF BREATH ,SINCE 20 DAYS
CHEST PAIN ,SINCE 20 DAYS
B/L PEDAL EDEMA , SINCE 4 DAYS
FACIAL PUFFINESS , SINCE 4 DAYS
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Ejection fraction (EF) is a measurement, expressed as a percentage, of how much blood the left ventricle pumps out with each contraction
1.Heart Failure with Reduced Ejection Fraction
Also called systolic heart failure, heart failure with reduced ejection fraction
It is the most common type of heart failure. It occurs when the left ventricle, the heart’s main pumping chamber, weakens and can’t pump blood effectively. This condition is also often called dilated cardiomyopathy.
2.Heart Failure with Preserved Ejection Fraction
In this condition, which is also called diastolic heart failure, the heart doesn’t relax properly, reducing the efficiency of the circulation of blood.
2.Why haven't we done pericardiocenetis in this pateint?
Pericardiocentesis is the most useful therapeutic procedure for the early management or diagnosis of large, symptomatic pericardial effusion and cardiac tamponade.Since this patient has no Cardiac tamponade(life-threatening slow or rapid compression of the heart due to increasing pericardial fluid) there is no need for pericardiocentesis
3.What are the risk factors for development of heart failure in the patient?
1.cigarette smoke can also cause CVD by changing your blood chemistry and causing plaque—a waxy substance comprised of cholesterol, scar tissue, calcium, fat, and other material to build up in the arteries, the major blood vessels that carry blood from your heart to your body. This plaque buildup can lead to a disease called atherosclerosis.
2.Alcoholic cardiomyopathy is a form of heart disease caused by alcohol abuse. Long-term alcohol abuse weakens and thins the heart muscle, affecting its ability to pump blood
4.What could be the cause for hypotension in this patient?
Low BP in HFrEF may have multiple origins such as low cardiac function, hypovolaemia (usually due to diuretics), treatment-related vasodilatation and altered vasoreactivity related to comorbidities such as diabetes.
SECOND CASE-
A 73 yr male patient teacher by occupation, resident of .............. presented to Opd with chief complaints of :
- PEDAL EDEMA ,SINCE 15 DAYS
- SHORTNESS OF BREATH, SINCE 4 DAYS
- DECREASED URINE OUTPUT ,SINCE 2 DAYS
Questions:
1.What are the possible causes for heart failure in this patient?
1.Alcoholic cardiomyopathy is a form of heart disease caused by alcohol abuse. Long-term alcohol abuse weakens and thins the heart muscle, affecting its ability to pump blood
2.High blood glucose from diabetes can damage your blood vessels and the nerves that control your heart and blood vessels
3.High blood pressure can strain your heart, damage blood vessels, and increase your risk of heart attack
2.what is the reason for anaemia in this case?
In the general elderly population, anemia is caused by nutritional deficiencies (primarily iron), chronic inflammation/CKD, or unexplained anemia of the elderly (a hypoproliferative anemia with blunted erythropoietin response)
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
When high blood sugar destroys nerves, they do not regenerate; thus many patients with diabetes are increasingly less sensitive to pain in their limbs. With this loss of sensation, patients don't feel developing blisters, infections, or existing wound changes. That means that wound healing is complicated not only by the fact that patients don't feel wounds as they occur, but they also have no pain to alert them that a wound is getting worse or infected.
4. What sequence of stages of diabetes has been noted in this patient?
- stage 1: defined as DCBD (dysglycemia-based chronic disease )insulin resistance;
- stage 2: defined as DCBD prediabetes;
- stage 3: defined as DCBD type 2 diabetes; and
- stage 4: defined as DCBD vascular complications, including retinopathy, nephropathy or neuropathy, and/or type 2 diabetes-related microvascular events.
- All these stages have been noted in this case.
A 52yr old male came to the OPD with the chief complaints of decreased urine output and shortness of breath at rest since one day.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Surgery for Inguinal hernia 10yrs ago. had On and Off pain at surgical site which aggravated since 3yrs.
Facial puffiness On and Off since 2-3yrs
HTN since 1yr. (Grade II i.e SOB on exertion).Shortness of breath Grade II (on exe
rtion) which progressed to Grade IV (at rest) 2 days back and Anuria.
Anatomical localisation :Heart (Atria)
Etiology :
Loss of Atrial contraction and Left atrial dilatation causes stasis of blood in the LA and may lead to Thrombus formation in the Left Atrial Appendage. This predisposes patients to stroke and other forms of systemic embolism.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1.Dobutamine injection is indicated when parenteral therapy is necessary for inotropicsupport in the short-term treatment of adults with cardiac decompensation due to depressed contractility resulting either from organic heart disease or from cardiac surgical procedures.In patients who have atrial fibrillation with rapid ventricular response, a digitalis preparation should be used prior to institution of therapy with dobutamine hydrochloride 4.Carvedilol is used alone or together with other medicines to treat high blood pressure
5.Acitrom - Treatment and prevention of Blood clots
6.Cardivas 3.125 Tablet is a medicine used to treat high blood pressure, heart-related chest pain (angina), and heart failure. It works by relaxing the blood vessels, so blood can flow more easily to the heart.
7.Dytor 10 mg is used to reduce the swelling (edema) caused by too much water in the body in people who have heart failure, liver disease, or kidney disease. This medicine is also used to treat high blood pressure.
8.Pan D capsule is used to treat GERD (Gastrointestinal reflux disease), not responding to pantoprazole alone. It helps in relieving symptoms such as heartburn, chest discomfort or acidity.
9.Taxim-O 200 tablet is used for the bacterial infection
10.HAI SC
Human Actrapid 40IU/ml Solution for Injection is a short-acting insulin used to treat type 1 and type 2 diabetes mellitus. It is used together with a healthy diet and regular exercise to control blood sugar levels after meals. This helps to prevent serious complications of diabetes like kidney damage and blindness.
11.Inj thiamine
To treat or prevent thiamine(B1) insufficiency
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Cardiorenal syndromes (CRS) describe concomitant bidirectional dysfunction of the heart and kidneys in which 1 organ initiates, perpetuates, and/or accelerates decline of the other. CRS are common in heart failure and universally portend worsened prognosis.
It is Type-4 CRS, also defined as chronic reno-cardiac disease, is characterized by cardiovascular involvement in patients affected by chronic kidney disease at any stage
4) What are the risk factors for atherosclerosis in this patient?
Hypertension since 1 yr
Cardiorenal syndrome type 4
5) Why was the patient asked to get those APTT, INR tests for review?
The partial thromboplastin time (PTT; also known as activated partial thromboplastin time (aPTT)) is a screening test that helps evaluate a person's ability to appropriately form blood clots. It measures the number of seconds it takes for a clot to form in a sample of blood after substances (reagents) are added. The PTT assesses the amount and the function of certain proteins in the blood called coagulation or clotting factors that are an important part of blood clot formation. The INR is found using the results of the prothrombin time (PT) test. This measures the time it takes for your blood to clot. The INR is an international standard for the PT.
FOURTH CASE-
A 67 year old female patient came to the OPD with C/O shortness of breath (SOB) since 1/2 hour.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
DM2 since 12 years
heartburn like episodes since a year
TB diagnosed 7 months ago
hypertension since 6 months
SOB since 1/2 hour.
Anatomical localisation:
Heart muscle
PRIMARY ETIOLOGY-
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1.Met XL 25 tablet is used to lower the raised blood pressure and various other heart-related conditions such as angina (chest pain), heart failure, preventing further complications.
2.Glimiprime M 2 Forte Tablet is a combination of two medicines: Glimepiride and Metformin. This medicine is used in the treatment of type 2 diabetes mellitus (DM). It improves blood glucose levels in adults when taken along with proper diet and regular exercise
3.Telma 20 tablet is an antihypertensive medicine that is used to treat high blood pressure and can also help in reducing other heart problems It acts by relaxing the blood vessels and leads to lower blood pressure
3) What are the indications and contraindications for PCI?
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)Non–ST-elevation acute coronary syndrome (NSTE-ACS)Unstable angina.Stable angina.Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)High risk stress test findings.CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.Absence of cardiac surgery backup.Hypercoagulable state.High-grade chronic kidney disease.Chronic total occlusion of SVG.An artery with a diameter of <1.5 mm.4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
People suffer complications including bleeding, blood clots, infection, heart rhythm disturbances and even death from heart attack if PCI is performed in a patient who does not need it.
It is associated with substantial morbidity and mortality given the large amount of subtended myocardium at risk
Over testing and over treatment can raise a person’s risk of cardiovascular death by as much as four times.
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Evolution of symptomatology:
Uncontrolled DM2 since 8 years
↓
3 days back Mild chest pain dragging type and retrosternal pain(radiated)
Anatomical localisation: Inferior wall of heart
Primary etiology: Diabetes type 2 (uncontrolled)
high blood glucose from diabetes can damage your blood vessels and the nerves that control your heart and blood vessels
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1.Aspirin indications
- Angina pectoris
- Angina pectoris prophylaxis
- Ankylosing spondylitis
- Cardiovascular risk reduction
- Colorectal cancer
- Fever
- Ischemic stroke
- Ischemic stroke: Prophylaxis
- Myocardial infarction
- Myocardial infarction: Prophylaxis
- Osteoarthritis
- Pain
- Revascularization procedures: Prophylaxis
- Rheumatoid arthritis
- Systemic lupus erythematosus
2.Atorvas
- pain or burning when you urinate,
- upper stomach pain,
- weakness,
- feeling tired,
- loss of appetite,
- dark urine,
3.Clopibb :peripheral vascular disease (blood circulation problems due to narrowing of blood vessels), recent heart attack or stroke, irregular heartbeats, and those who have undergone certain heart procedures like stenting. It is also used in combination with some other medicines for the treatment of heart attack and some types of heart-related chest pain (unstable angina).4.HAI SC
Human Actrapid 40IU/ml Solution for Injection is a short-acting insulin used to treat type 1 and type 2 diabetes mellitus. It is used together with a healthy diet and regular exercise to control blood sugar levels after meals. This helps to prevent serious complications of diabetes like kidney damage and blindness.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Repeat PTCA provides a valuable, safe and cost-effective way of management for recurrence of stenosis after initially successful angioplasty. It increased the percent of patients with documented long-term success of angioplasty
——————————————————————————————————————
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
The patient has decreased Urine output since 3 days. This might have been due to Fluid loss in the patient.
Decreased preload
↓
SOB occured due to decreased cardiac output
↓
IV fluids administered
there is increase in preload
↓
SOB decreased due to better cardiac output
2. What is the rationale of using torsemide in this patient?
Torsemide is used to treat edema (fluid retention; excess fluid held in body tissues) caused by various medical problems, including heart, kidney, or liver disease
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Treatment for UTI
Rationale - used for any bacterial infection .
GASTROENTEROLOGY(and PULMONOLOGY)-
FIRST CASE-
A 33 YEAR OLD MAN WITH PANCREATITIS, PSEUDOCYST AND LEFT BRONCHO-PLEURAL FISTULA
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
5 yrs back when he had painabdomen & vomitings
stopped taking alcohol as advised by the physician and was symptom free for nearly 3 yrs.
* (5-6 episodes in the past 1 year) again started taking alcohol recurrent episodes of pain abdomen & vomiting
past 20 days he had increased amount alcohol consumption (5 bottles of toddy per day)
alcohol 1 week back following which he again had pain abdomen & vomiting from 1 week and fever from 4 days.
fever from 4 days. constipation since 4 days burning micturition since 4 days,
Anatomical localisation:
Pancreas and left lung
Primary etiology:
Alcohol and its metabolites produce changes in the acinar cells, which may promote premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury. Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by cytokines and growth factors released during alcohol-induced pancreatic necroinflammation. Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
1) ING. MEROPENAM ; TID for 7 days Meropenem ( broad spectrum Carbepenem ) an antibiotic.
2) ING. METROGYL 500 mg IV TID for 5 days has METRONIDAZOL( Nitroimidazole drug ) an antibiotic
3) ING. AMIKACIN 500 mg IV BD for 5days. It is an Aminoglycoside antibiotic
All these above drugs are used as antibiotics to control infection and ; to prevent septic complications of acute pancreatit
4) TPN ( Total Parenteral Nutrition )Method of feeding that by passes gastrointestinal tract.Fluids are given to vein , it provides most of the nutrients body needs.TPN has proteins, carbohydrates, fats, vitamins, minerals.
5) IV NS / RL at the rate 12l ml per hour
Given for fluid replacement ie., treat dehydration
6) ING. OCTREOTIDE 100 mg SC , BD
It is a Somatostatin long acting analogue.It is used here to decrease exocrine secretion of pancreas and it also has anti- inflammatory & cytoprotective effects.
7) ING. PANTOP 40 mg IV , OD has PANTOPRAZOLE ( Proton Pump Inhibitor) used for its anti pancreatic secretory effect.
8) ING. THIAMINE 100 mg in 100 ml NS IV , TID
It is B1 supplement. It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplemention is necessary.
9) ING. TRAMADOL in 100 ml NS IV , OD It is an opioid analgesic, given to releive pain
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
Acute pancreatitis in its severe form is complicated by multiple organ system dysfunction, most importantly by pulmonary complications which include hypoxia, acute respiratory distress syndrome, atelectasis, and pleural effusion. The pathogenesis of some of the above complications is attributed to the production of noxious cytokines
2) Name possible reasons why the patient has developed a state of hyperglycemia.
Hyperglycemia develops rather often in the early phase of acute pancreatitis, mainly in patients with severe disease . This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress or the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells .
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Elevated liver enzymes in the setting of acute pancreatitis point toward choledocholithiasis as the cause, with an alanine aminotransferase greater than three times the upper limit of normal having a positive predictive value of 95% for gallstone pancreatitis .
In heavy drinkers, serum GGT, AST, ALT, ferritin and albumin were all significantly higher than in moderate drinkers or abstainers
4) What is the line of treatment in this patient?
clinicians employ goal-directed fluid therapy with either normal saline or lactated Ringers, give timely analgesics and antiemetics, and replete electrolytes as needed. The current recommendations are also to initiate feeding trials within 24 hours of disease onset instead of keeping the patient nill per mouth (NPO). There are no clear indications for the type of diet, but typically small low-fat, soft or solid meals correlate with shorter hospital stays than starting a clear liquid diet with slow advancement to solid meals. Enteral feeds via a feeding tube are preferred to total parenteral nutrition in patients unable to tolerate PO
——————————————————————————————————————
Possible Questions :-
1) what is the most probable diagnosis in this patient?
Ruptured liver abscess
2) What was the cause of her death?
Spontaneous gas-forming pyogenic liver abscess (GFPLA) is a rare complication with a high fatality rate in spite of aggressive management. Clinical spectrum of GFPLA can mimic hollow viscus perforation as it usually accompanied by pneumoperitoneum and peritonitis.
3) Does her NSAID abuse have something to do with her condition? How?
NSAIDs are absorbed completely and undergo negligible liver metabolism.
——————————————————————————————————————
5) Nephrology (and Urology)
1. What could be the reason for his SOB ?
Since the patients creatinine levels are very high, functioning of the kidney is reduced. This causes for the accumulation of fluid in the lungs and thus causes SOB
2. Why does he have intermittent episodes of drowsiness ?
In healthy individuals, sleep is accompanied by a decrease in sympathetic activity and an increase in vagal tone that leads to a nocturnal dipping of blood pressure
In any kind of kidney related problem it exhibit sympatho-vagal imbalance due to baroreceptor reflex function impairment in which there is hyperactivity of the sympathetic nervous system and decreased vagal tone
3. Why did he complaint of fleshy mass like passage in his urine?
Creatinine is a normal waste product that the body produces every day during muscle movements and when digesting meat.
When creatinine is very high it probabaly means that high waste product of muscle is being formed and this might result in fleshy mass like passage
4. What are the complications of TURP that he may have had?
Transylurethral resection of prostate (TURP)
1.Bladder injury
2.Bleeding
3.Blood in the urine after surgery
4.Electrolyte abnormalities
5.Infection
6.Loss of erections
7.Painful or difficult urination
8.Retrograde ejaculation (when ejaculate goes into the bladder and not out the penis)
——————————————————————————————————————
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
2. Why doesn't the child have the excessive urge of urination at night time ?
Since the child doesn’t have excessive urge of urination at night but at day there might be a psychiatry related condition
1. Psychosomatic disorder
2. Undiagnosed anxiety disorder
3. How would you want to manage the patient to relieve him of his symptoms?
A)If the cause is an overactive bladder, a medication known as an anticholinergic may be used. These prevent abnormal involuntary detrusor muscle contractions from occurring in the wall of the bladder
B)To treat attention deficit hyperactivity disorder:For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.
1.Methylphenidate A stimulant and a medication used to treat Attention Deficit Hyperactivity Disorder. It can make you feel very ‘up’, awake, excited, alert and energised, but they can also make you feel agitated and aggressive. They may also stop you from feeling hungry.
2.Amphetamine belongs to a class of drugs known as stimulants. It can help increase your ability to pay attention, stay focused on an activity, and control behavior problems. It may also help you to organize your tasks and improve listening skills.
——————————————————————————————————————
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology)
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
1.The patient is a known case of Retroviral Disease but she was on her ART since 2 months. There might be a possible chance that her negligence to treat RVD is the cause of her Tracheo esophageal and also TB.
2.Physical finding
According to CECT there is a fistulous communication between left main bronchi and mid thoracic oesophagus few centimetres below carina
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Immune reconstitution inflammatory syndrome (IRIS) is a condition seen in some cases of AIDS or immunosuppression, in which the immune system begins to recover, but then responds to a previously acquired opportunistic infection with an overwhelming inflammatory response that paradoxically makes the symptoms of infection worse. The suppression of CD4 T cells by HIV (or by immunosuppressive drugs) causes a decrease in the body's normal response to certain infections. Not only does this make it more difficult to fight the infection, it may mean that a level of infection that would normally produce symptoms is instead undetected (subclinical infection). If the CD4 count rapidly increases (due to effective treatment of HIV, or removal of other causes of immunosuppression), a sudden increase in the inflammatory response produces nonspecific symptomssuch as fever, and in some cases a worsening of damage to the infected tissue 7) Infectious disease and Hepatology:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ? What could be the cause in this patient ?
Like any other alcoholic drink, excessive toddy (8.1%)drinking can damage the liver.Even the alcohol content is less than that of wine, the patient has been drinking it since 30 years . Therefore it is the major predisposing factor
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
A)There can be various mechanisms by which toddy could influence EH (Entamoeba Histolytica) virulence. The resident microbial flora in human colon is an important determinant of survival and virulence in EH.
Alcohol consumption is known to induce intestinal bacterial dysbiosis, which may in turn alter the activity of EH. Undistilled local alcoholic beverages contain a large number of microorganisms that might have more propensity to cause intestinal dysbiosis.
EH lacks mitochondria and obtains its energy from the fermentation of glucose. EH alcohol dehydrogenase 2 (EHADH2) is a key enzyme in this pathway.Thus, expression of EHADH2 is required for the growth and survival of EH trophozoites in human.
B)alcohol suppresses the function of Kupffer cells in the liver, which has the important role of clearing the amoeba. This leads to pathogenic invasion leading abscess formation
3. Is liver abscess more common in right lobe ?
Right lobe is more significant part with more blood supply. Therefore liver abscess is more common
4.What are the indications for ultrasound guided aspiration of liver abscess ?
- Presence of a left-lobe abscess more than 10 cm in diameter.
- Impending rupture and abscess that does not respond to medical therapy within 3-5 days.
- If the abcess is large ( 5cm or more) because it has more chances to rupture.
———————————————————————————————————
QUESTIONS:
1) Cause of liver abcess in this patient ?
The patient is occasional toddy drinker which has high amount of Entamoeba histolytica. This causes liver abscess by suppressing the function of Kuffper cells.Therefore Toddy is most probable cause of Liver abscess in this patient
2) How do you approach this patient ?
Hematology:
1.Common hematological finding being LEUCOCYTOSIS , indicating inflammation or infection
2.Anemia may be present , or not.
Chemistry:
Elevated liver enzymes such as AST,ALP are noted .
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
1.INJECTION. ZOSTUM 1.5 gm IV BD (twice daily) Zostum is a combination of drugs - SULBACTUM (pencillin) & CEFOPERAZONE(cephalosporin) [Antibiotic]: It is used here to treat if any bacterial cause ( since we can’t take the risk relying on only anti amoebic therapy)
2.INJECTION. METROGYL 500mg IV TID ( thrice daily )Metrogyl has the drug called METRONIDAZOLE[Antibiotic]: For amoebic cause
4.INJECTION. OPTINEURIN 1amp in 100 ml NS( Normal Saline) IV OD is a multivitamin drug { A combination of B1,B2, B3, B5,B6, B12 } given here as a supplement
5.TAB. ULTRACET 1/2 QID( four times a day)is a combination of drugs - TRAMADOL(opiod analgesic) and ACETAMINOPHEN (analgesic and antipyretic) : Given for pain and fever
6.TAB. DOLO 650 mg SOS (if needed) given for fever and pain
* Here ; due to medical therapy his symptoms subsided and clearly we can see it in usg reports ( liquefaction) meaning abcess responded to our medical therapy.
4) Is there a way to confirm the definitive diagnosis in this patient?
Apart from serological examination which is positive in 94% of the cases..Further confirmation can be done by using Ultrasonography but these are not commonly used
——————————————————————————————————————
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology)
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Evolution of symptomatology
2 years back Hypertension and acute kidney disease
↓
18-4-21 Fever with chills and rigors(relieved on medication)
↓
21-4-21 similar complaints (relieved on medication)
↓
28-4-21 Generalised weaknes,facial puffiness,peri orbital oedema and drowsy
↓
4-5-21 presented to the hospitalon the morning
↓
In the evening-Serous discharge from left eye(blood tinged)
↓
5-5-21 referred to ENT
Blackish discolouration on medial canthus and bloody discharge
Oral cavity-Foul smelling, blackish each are tending from hardpalate towards upper lip
Anatomical localisation :
Medial canthus of left , Oral cavity and hardpalate, left nasal cavity and left frontal & temporal lobes
Primary etiology :
Mucormycetes, the group of fungi that cause mucormycosis, are present throughout the environment, particularly in soil and in association with decaying organic matter, such as leaves, compost piles, and animal dung. 1 They are more common in soil than in air, and in summer and fall than in winter or spring. 2-4 Most people come in contact with microscopic fungal spores every day, so it’s probably impossible to completely avoid coming in contact with mucormycetes. These fungi aren’t harmful to most people. However, for people who have weakened immune systems, breathing in mucormycete spores can cause an infection in the lungs or sinuses which can spread to other parts of the body.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
1.Itraconazole acts by inhibiting the fungal cytochrome P-450 dependent enzyme lanosterol 14-α-demethylase. When this enzyme is inhibited it blocks the conversion of lanosterol to ergosterol, which disrupts fungal cell membrane synthesis. Itraconazole exhibits fungistatic (slows the growth) activity against yeast-like fungi and fungicidal (kills the fungus) activity against Aspergillus spp.
2.Amphotericin B binds with ergosterol, a component of fungal cell membranes, forming pores that cause rapid leakage of monovalent ions (K+, Na+, H+ and Cl−) and subsequent fungal cell death
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Low oxygen, diabetes, high iron levels, immunosuppression, as well as several other factors including prolonged hospitalisation with mechanical ventilators, creates an ideal milieu for contracting mucormycosis,
Contamination in pipes of the oxygen cylinders
unhygienic masks" and poorly ventilated rooms could be a contributing factor
history of exhibiting poor hygienic practices, including wearing unwashed masks for a long time.
irrational use of steroids
Mucormycosis is more common among people whose immunity has lowered due to COVID, diabetes, kidney disease, liver or cardiac disorders, age-related issues, or those on medication for auto-immune diseases like rheumatoid arthritis.
——————————————————————————————————————
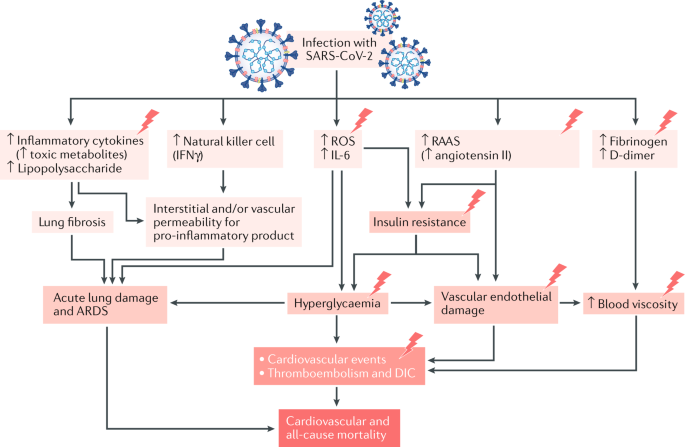
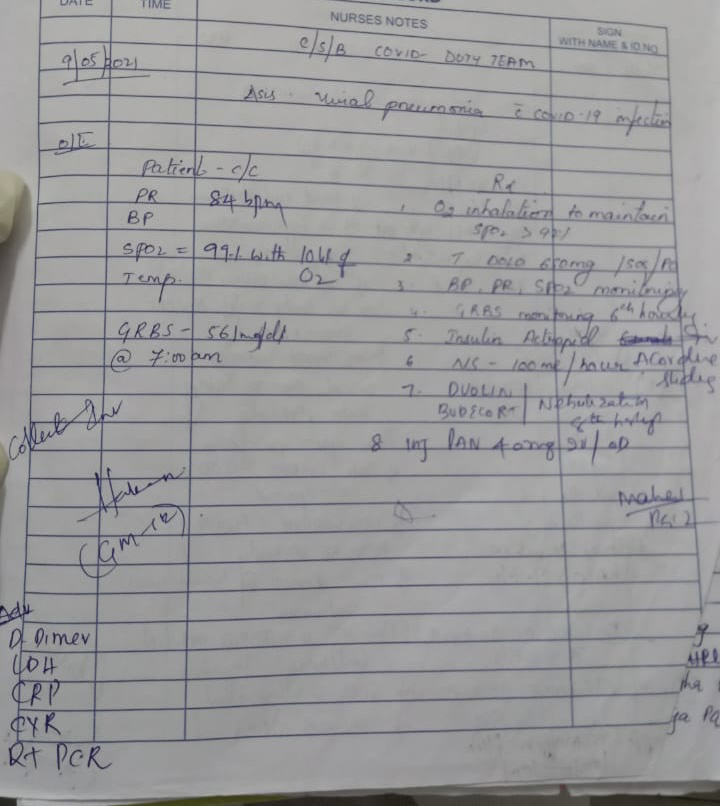
9) Infectious Disease (Covid 19)
Here is my attempt to solve cases in regarding to understand the topic of SARS COV-2 (COVID -19) to develop my competency in reading and comprehending clinical data including history,clinical data including history,clinical findings, investigations and diagnosis and come up with a treatment plan.
Master chart -
Experimental learning-






Comments
Post a Comment