40yrs old man with pleural effusion
FINAL EXAMINATION CASE REPORT :
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current based inputs.
Roll no -1701006042
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Case presentation:
A 40 years old Male, resident of bhongir, painter by occupation presented to OPD with
CHIEF COMPLAINTS:
- Shortness of breath since 7 days
- Chest Pain on left side since 5days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 7days back then developed shortness of breath which was
- insidious in onset
- gradually progressive (grade I to grade II according to MMRC)
- Chest pain:
non radiating
nature: pricking type - loss of weight(about 10kgs in past 1yr)
- loss of appetite
- wheeze
- palpitations
- chest tightness
- cough
- hemoptysis
PAST HISTORY:
- Diabetes Mellitus 3 yrs back (on medication- Metformin 500mg, Glimiperide 1mg)
PERSONAL HISTORY:
- Mixed diet
- sleep is adequate ( but disturbed from past few days)
- loss of appetite is present
- bowel and bladder movements are regular
- He used to Consume
- Alcohol stopped 20years back ( 90ml per day)
Smoking from past 20years (10 cigarettes per day) but stopped 2years back.
FAMILY HISTORY:
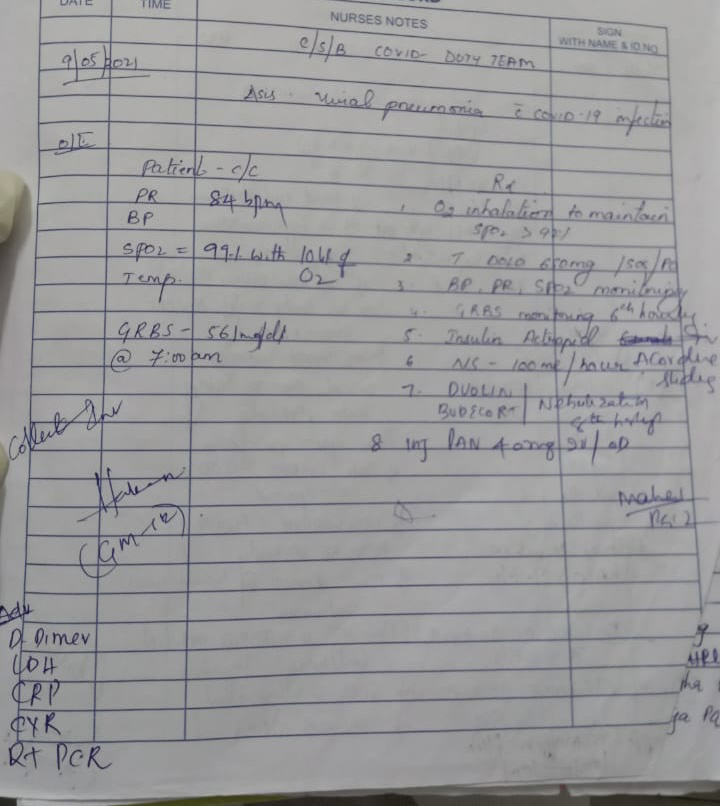
VITALS:
Pulse rate : 139beats/min
BP : 110/70 mm Hg
RR : 45 cpm
SpO2 : 91% at room air
GRBS : 201mg/dl
SYSTEMIC EXAMINATION:
RESPIRATORY EXAMINATION:
INSPECTION:
Shape of chest is elliptical,
B/L asymmetrical chest,
Trachea in central position,
Expansion of chest- Right- normal, left-decreased,
Use of Accessory muscles is seen
PALPATION:
All inspectory findings are confirmed,
No tenderness, No local rise of temperature,
trachea is deviated to the right,
Measurement:
AP: 24cm
Transverse:28cm
Right hemithorax:42cm
left hemithorax:40cm
Circumferential:82cm
Tactile vocal fremitus: decreased on left side ISA, InfraSA, AA, IAA
PERCUSSION:
Dull note present in left side ISA, InfraSA, AA, IAA
AUSCULTATION:
B/L air entry present, vesicular breath sounds heard,
Decreased intensity of breath sounds in left SSA,IAA,
Absent breath sounds in left ISA
CVS EXAMINATION:
S1,S2 heard
No murmurs. No palpable heart sounds.
JVP: normal
Apex beat: normal
PER ABDOMEN:
Soft, Non-tender
No organomegaly
Bowel sounds heard
no guarding/rigidity
CNS EXAMINATION:
No focal neurological deficits
Gait- NORMAL
Reflexes: normal
PROVISIONAL DIAGNOSIS:
INVESTIGATIONS:
DB: 0.74mg/dl
AST: 24IU/L
ALT: 09IU/L
ALP: 167IU/L
TP: 7.5gm/dl
ALB: 3.29gm/dl
INTERPRETATION: As 2 values are greater than the normal we consider as an EXUDATIVE EFFUSION.










Comments
Post a Comment