COVID CASE REPORT
E.RISHITHA REDDY
MEDICINE CASE DISCUSSION
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 42YEAR OLD FEMALE PATIENT WITH A HISTORY OF SOB-
Following is the view of my case : (Admitted on 13/05/21 , 9 pm)
CASE REPORT-
A 42year old female patient came with a history of high grade
fever 10 days back , SOB since 3days on exertion , cough
productive since 2days and has chest pain since 3days
HISTORY OF PRESENTING ILLNESS-
Patient complained that she has a high grade , intermittent
fever 10 days back. Then she developed SOB which is of
sudden in onset and progressive on exertion . SOB is
associated with chest pain which is intermittent since 2 days
On exertion.She also has cough since 2 days. It is associated
with sputum in small quantity.
And RAT was done in COVID OPD and tested positive.
Her SpO2 levels are 82% on RA
Pulse rate -124bpm
She was advised admission
PAST HISTORY-
She is a known case of hypothyroidism since 4 years. And on
Tab. Thyronorm 100mcg O.D
SURGICAL HISTORY-
She has a history of hysterectomy 20years back.
PERSONAL HISTORY :
Diet - mixed
Appetite - decreased
Bowel and bladder habits - regular
Sleep - inadequate
FAMILY HISTORY-
No significant family history.
GENERAL EXAMINATION-
The patient is conscious coherent well oriented to time place
and person and sitting comfortably on bed moderately built
and well nourished.
PALLOR- absent
ICTERUS -absent
CYANOSIS- absent
CLUBBING- absent
LYMPHADENOPATHY - absent
EDEMA- absent
VITALS-
Temperature- Afebrile
PR-94bpm
BP- 120/90mm hg
SpO2- 99% with 5litres of O2
SYSTEMIC EXAMINATION-
CVS- S1 S2 heard . No added Murmurs
PA- soft and non tender , No organomegaly
CNS-intact
Respiratory system- Normal vesicular breath sounds heard
INVESTIGATIONS-
CBP-
Hb-12.7gm%
TC-5,700
DC-N80 L15 E 02 M03 B00
DLC-1.5lakh/mm3
D-dimer-10ng/ml
Serology-
LDH-571
CRD-2.4mg/dl(positive)
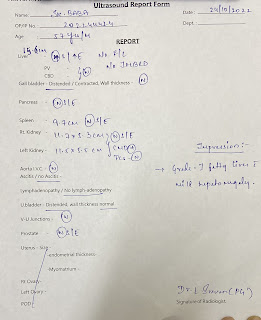
HRCT-
CT score-16/25
LFT AND RFT-
On 13/5/21-
On 14/5/21-
TRP graphic chart-
PROVISIONAL DIAGNOSIS-
COVID-19 pneumonia with a known case of hypothyroidism.
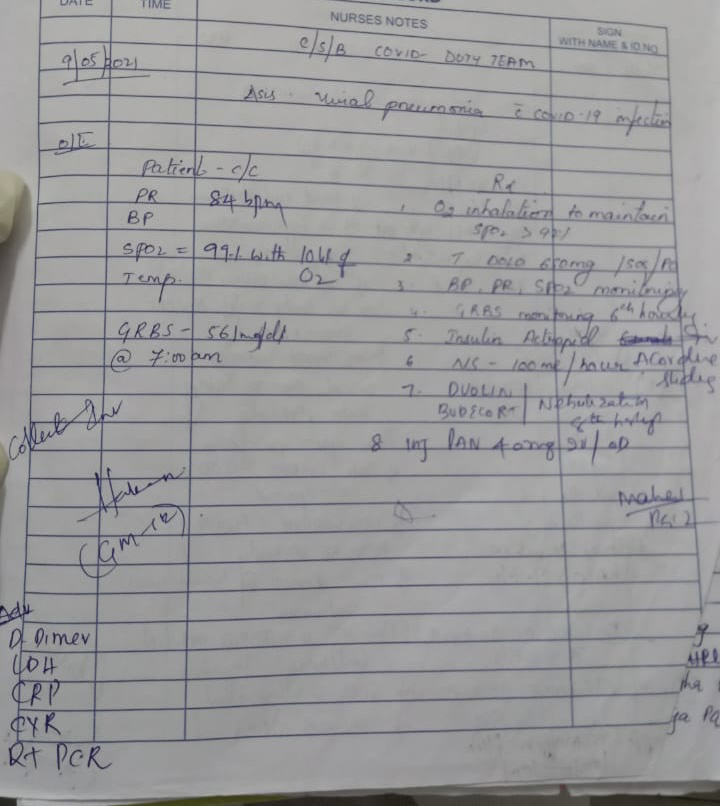
Rx-










Comments
Post a Comment