Rishitha Reddy
- Get link
- X
- Other Apps
COVID CASES MAY-

Link to Masterchart on COVID-19
9) Covid cases
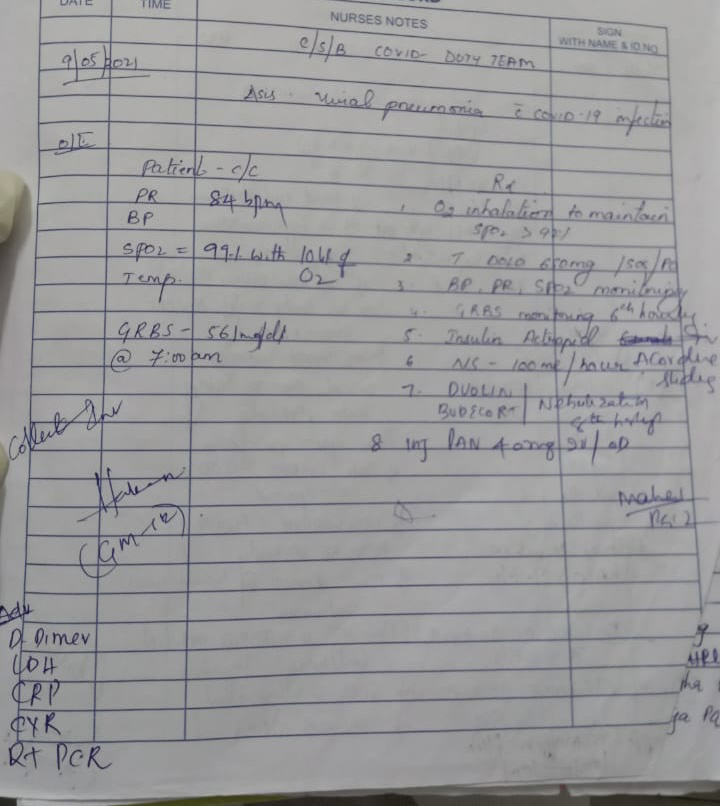
1) Covid 19 with co morbidity (Pulmonology/Rheumatology)
https://nikhilasampathkumar.
2) Covid 19 with Diabetes
3) Covid 19 Severe
noradrenaline, is a medication used to treat people with very low blood pressure. Noradrenaline is a vasoconstrictor that predominantly stimulates α1 receptors to cause peripheral vasoconstriction and increase blood pressure.It also has some β1 receptor agonist activity that results in a positive inotropic effect on the heart at higher doses.
2. What is the reason behind testing for LDH levels in this patient?
LDH is an intracellular enzyme found in cells in almost all organ systems, which catalyzes the interconversion of pyruvate and lactate, with concomitant interconversion of NADH and NAD+.Lactate dehydrogenase (LDH) is one such biomarker of interest, especially since elevated LDH levels have been associated with worse outcomes in patients with other viral infections in the past. It is estimated that if there was a >6-fold increase in odds of severe disease and a >16-fold increase in odds of mortality in patients with elevated LDH.
3. What is the reason for switching from BiPAP to mechanical ventilation with intubation in this patient? What advantages did it provide?
BiPap may not be a good option if your breathing is very poor. It may also not be right for you if you have reduced consciousness or problems swallowing
Therefore patient might have got shifted to Mechanical ventilation
Advantages of Mechanical ventilation
- The patient does not have to work as hard to breathe – their respiratory muscles rest.
- The patient's as allowed time to recover in hopes that breathing becomes normal again.
- Helps the patient get adequate oxygen and clears carbon dioxide.
- Preserves a stable airway and preventing injury from aspiration.
4) Covid 19 Mild
HARMS OF HOSPITALIZATION
Patients with COVID-19 had almost 19 times the risk for acute respiratory distress syndrome (ARDS) than did patients with influenza, and more than twice the risk for myocarditis,deep vein thrombosis ,pulmonary embolism, intracranial hemorrhage, acute hepatitis/liver failure, bacteremia,and pressure ulcers .
The risks for exacerbations of asthma and chronic obstructive pulmonary disease were lower among patients with COVID-19 than among those with influenza.
The percentage of COVID-19 patients who died while hospitalized (21.0%) was more than five times that of influenza patients (3.8%), and the duration of hospitalization was almost three times longer for COVID-19 patients.
——————————————————————————————————————5) Covid 19 and comorbidity (Altered sensorium, azotemia, hypokalemia)
2.After prolonged periods of mechanical ventilation in the ICU.
Her grades was 12/25 according to her ct scan.(moderate)
What is the ideal day to start steroids in a patient with mild elevated serum markers for COVID ?
Ideal day for steroid administration is after the 8th day (early of pulmonary phase)of symptoms, when the virus is very low replecable and inflammatory response is about to settle down
What all could be the factors that led to psychosis in
It can be due to any of the following reasons:
1.high dose corticosteroid use
2.Prolonged hospital stay
Severe inflammatory changes in lungs in case of covid pneumonia.
•Delayed recovery of the patient .
Since elevated blood sugar levels favors the virus growth and multiplication.
High LDH levels
Extremely high levels of LDH could indicate severe disease or multiple organ failure. Because LDH is in so many tissues throughout the body, LDH levels alone won't be enough to determine the location and cause of tissue damage.
The pneumonia that COVID-19 causes tends to take hold in both lungs. Air sacs in the lungs fill with fluid, limiting their ability to take in oxygen and causing shortness of breath, cough and other symptoms.While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID-19 can be severe. Even after the disease has passed, lung injury may result in breathing difficulties that might take months to improve.This might be the cause for persistent hypoxia in this patient
——————————————————————————————————————
2.Indication: At admission: pre-meal BG: ≥180 mg/dl or post-meal BG ≥250 mg/dl
A. Total daily dose (TDD) = 0.4 units/kg/day (age > 65 yr, nephropathy or liver disease, use 0.2 units/kg/day)
B. Total daily dose is divided equally into 4 doses (25% each): 3 doses are for bolus insulin (Regular insulin 30 min before breakfast, before lunch and before dinner) and 1 dose for basal insulin (Inj. NPH insulin at bed time/ 2 hours after dinner).If pre-meal BG value is 140 to 180 mg/dl and/or post-meal BG value is 180 to 250 mg/dl → consult endocrinologist/physician for OAD optimization
5. What is thrombophlebitis fever? Thrombophlebitis is when a blood clot Any veins and slows the blood flow in the vein. It may be due prolonged use of IV cannula. Due to inflammatory reaction, fever occurs.
There is no need to stop infusion to control Theombophlebitis. Instead change the IV cannula to opposite or another site. If there is pain at that site use aspirin or ibuprofen
——————————————————————————————————————As it is said, not all the patients who are given steroids might land up into Steroid induced Diabetes. Hence Oral hypoglycaemics might not have been prescribed
——————————————————————————————————————The exact pathogenesis of pleural effusion due to SARS-CoV-2 pneumonia is not known. However, patients have significantly increased inflammatory markers, which may signify an increase in capillary and endothelial dysfunction leading to exudation of fluid into the pleural space. Only 40% of pleural effusions were lymphocytic predominant (lymphocytes >50% of nucleated cells), lower than seen in other viral infection-related pleural effusions such as avian influenza.This finding can be explained by relative lymphopenia seen in patients with SARS-CoV-2 infection. Majority (3/5,60%) of effusions were hemorrhagic (RBC >100,000 per mm3) ,While it is possible that intrapleural bleeding could reflect a procedural complication in patients receiving systemic anticoagulation, anticoagulants were held prior to drainage. Moreover, most of these patients were on steroids, which can explain low eosinophils in the pleural space.
It can also be hypothesized that sanguineous pleural effusion in SARS- CoV-2 may be the result of endothelial dysfunction-related microthrombi from underlying inflammation that causes foci of hemorrhage in the lung parenchyma extending into the pleura.
——————————————————————————————————————
4. What other differential diagnoses could be drawn if the patient tested negative for covid infection?
D-dimer (or D dimer) is a fibrin degradation product (or FDP), a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis.
1.venous thromboembolism (VTE), which can present as either deep vein thrombosis (DVT) or pulmonary embolism (PE). 2. pro-coagulant state
——————————————————————————————————————
Consuming excessive amounts of alcohol could cause damage to immune cells in the lungs and upper respiratory system which in turn can increase the risk of developing diseases such as tuberculosis, pneumonia ,respiratory distress syndrome and make the lung more susceptible to virus entry
——————————————————————————————————————
COVID-19 associated ischemic strokes are more severe with worse functional outcome and higher mortality than non-COVID-19 ischemic strokes.
——————————————————————————————————————
The patient is a Diabetic since 7 years .As a result High blood glucose can damage the blood vessels in your kidneys. When the blood vessels are damaged, as a result the waste products start accumulating. Thus causing Chronic kidney disease/ Diabetic kidney disease
- Get link
- X
- Other Apps



Comments
Post a Comment